Researchers around the world are seeking to identify techniques that use nanoparticles in the treatment of disease. Such particles are about 100 nanometres – one thousandth of a millimetre – in diameter, and within them researchers are inserting large numbers of even smaller drug molecules.
Optimism for this approach in the treatment of various forms of cancer has been particularly great.
“We’ve observed that blood vessel walls in cancer tumours in mice have larger pores than the same vessels in healthy tissue”, says SINTEF researcher Sjoerd Hak. “If we inject nanoparticles into the blood, the pores make it easier for them to escape from the vessels and enter the tumour”, he says.
“In healthy tissue, where the blood vessels are intact, the nanoparticles cannot escape”, Hak tells Gemini.
Knowing this makes it easier to target the drugs on their desired destinations, and we can also limit the volume of drugs reaching parts of the body where they may cause harm.

Research Scientist Sjoerd Hak at SINTEF
However, nanomedicine faces a major problem. Our immune systems do not welcome small and unfamiliar foreign bodies.
A virus or a drug?
“The nanoparticles are about the same size as a virus and are normally made up of molecules that do not belong naturally in the blood. This means that the body will discover them and remove them”, explains Hak.
As a result, the nanoparticles will not be present in the blood for long enough to release an adequate dose of drugs to the target tumour.
“Much of our research has been focused on developing particles that can prolong their presence in the blood”, says Hak. “We’ve had some level of success, but drug uptake by tumour tissue still remains limited. In mice, we’ve achieved a lot of excellent results, but the effect continues to remain somewhat limited in humans”, he says.
As with so many other technologies prefixed with ‘nano-’, it is taking some time for nanomedicine to live up to the expectations it generated a decade or two ago.
“In relation to the extent of this field of research, very little has been achieved in terms of clinical treatments. But we will get there – I’m convinced of that”, says Hak.
In the meantime, he and his colleagues are testing an alternative route to the tumours for the nanodrugs. Instead of fighting against the immune system, the new approach is to team up with it and play along.
About the project:
Project name: ‘From evading to embracing immune cells – Development of neutrophil-targeted anti-cancer nanomedicine’
Project Manager: Sjoerd Hak, SINTEF
Participants: SINTEF and NTNU
Project period: 2021–2024
Funded by the Research Council of Norway (project no. 314984)
The aim of the project is to develop nanoparticles that are taken up by specific immune cells that play a damaging role in the development of cancerous tumours.
Scientific publication:
Jeffrey Momoh, Sjoerd Hak et al.: Intravital microscopy for real-time monitoring of drug delivery and nanobiological processes. In Advanced Drug Delivery Reviews, October 2022.
Aggressive immune cells
It is very difficult to prevent nanoparticles from being consumed by immune cells. Such cells are specialists in seeking out and removing foreign bodies. At the same time, our knowledge about the roles that these cells play has improved considerably, and a number of new treatments have been developed in the field of what we call immunotherapy.
“We’re trying to combine these two aspects as part of our research – and we’re not the only ones”, says Hak. “There are many researchers around the world who have realised this and who are trying to exploit interactions involving immune cells”, he says.
“Our intention is to use the body’s own defence mechanisms to attack cancerous tumours. We’re not necessarily targeting the cancer cells directly, but we want to make conditions less favourable for their growth and development”, explains Hak.
Targeting the drugs directly at the cancer cells is not the most important thing. The key objective here is what the drugs do when they interact with the immune cells and the immune system.
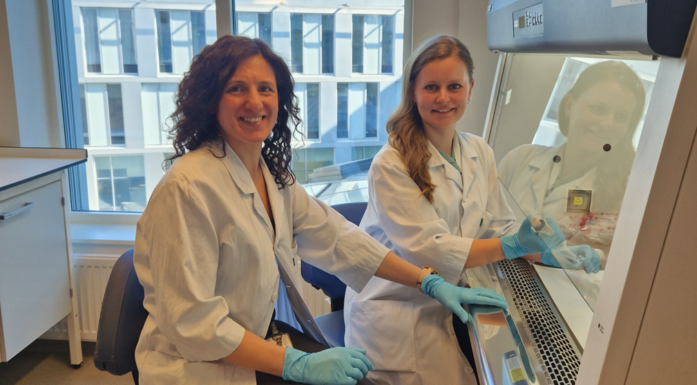
Project participants: Camilla Wolowczyk (right) is a post-doc student working with phagocyte targeting, pictured here with research scientist Miriam Giambelluca from NTNU.
What’s going on in living tumours
In order to achieve this, the researchers need more knowledge about what actually happens to the nanoparticles and the drug molecules they are carrying. One of the techniques they are using is called intravital microscopy.
“Intravital microscopy involves taking film and images of living tumours in mice under a microscope”, says Hak. “This enables us to look at individual cancer cells and examine the blood vessel walls”, he explains.
The nanoparticles are too small to be identified in isolation but, by making them self-illuminating, we can follow their movements.
“They’re too small to see individually, even under a microscope, but we know where they are because we can detect their fluorescence”, says Hak.
The video above shows intravital microscopy images of nanoparticles being taken up in the body.
“We can see the immune cells moving around and that they have taken up large numbers of fluorescent particles”, says Hak. “Within the tumour, we can see cells that are quite immobile and which have also taken up particles”, he explains.
“We can see that some immune cells actually seem to be responsible, at least in part, for the uptake of particles in the tumour. It is not possible to observe this using techniques other than intravital microscopy”, says Hak.
It is not possible to obtain this kind of information using MRI or PET scanning techniques.
“Intravital microscopy has provided us with a better mechanistic understanding of how these particles accumulate in a tumour”, says Hak.
Changing the behaviour of immune cells
Researchers have demonstrated that it is in fact possible to get the particles into the immune cells within the tumour. The next step is to identify the correct drug and, not least, ensure that it will have a therapeutic effect. The natural response of the immune cells is to attempt to destroy the nanoparticles, and they are more than adequately equipped to achieve this.
“The immune cells attempt to break down the particles”, says Hak. “They contain a variety of enzymes and acids, as well as dedicated spaces, or compartments, where they send material for destruction”, he says.
These immune cells are what researchers call phagocytes, from the Greek meaning ‘eating cells’. Hak and his colleagues are looking to manipulate these phagocytes so that they change their behaviour.
“We’re working with two different drugs that we’ve encapsulated within the nanoparticles and are now trying to see what kinds of effects these have on the immune cells”, explains Hak.
They are targeting the phagocytes because they can ‘change sides’ and work to the benefit of the tumour rather than against it.
“We know that these cells play key roles when a tumour grows and develops. The tumour succeeds in deceiving them into working for its benefit”, says Hak.
“What we’re trying to do is manipulate or shut down the functions of cells that are working for the tumour”, he says.
Promising test results in mice
In effect, this means that researchers are attempting to increase the immune cells’ uptake of nanoparticles. This is the complete opposite of what medical research has been working to achieve for many years. At present, they are looking into how the process works in isolated human immune cells and in mice with breast cancer.
“We completed the first therapeutic experiments a few weeks ago and the results are very interesting”, says Hak. “But there’s a lot more work to do before we can draw any conclusions. “It will take time to identify exactly how we go about things, as well as what concentrations and incubation times are the most appropriate”, he explains.
“There is a lot we have to find out before we can say that this technique works”, says Hak. “Perhaps we’ll find out that it doesn’t work at all using the two drugs we’ve selected. In that case, we may have to start again from scratch with new drugs”, he says.
A key bottleneck in the process, not only for this project, but for the entire field of nanomedicine, is trying to persuade the particles carrying the drugs to leave the compartments where the cells have sent them for destruction.
“It looks as if the molecules that we are using are able to escape”, says Hak. “Our initial results are confirming this, so I believe that we will succeed, although it’s too early yet to say for sure”, he says.
Opportunities for innovative approaches
As with all other medical research, many small steps have to be taken before we can apply new treatment methods to patients. Sjoerd Hak sees this project as part of a much bigger picture.
“Of course it would be very exciting if we were to identify a treatment that worked so well that it justified further research into precisely the same nanodrug that we are making.”, he says.
“But from a personal point of view, I’m more interested in demonstrating that we can achieve therapeutic effects using this technique. After all, it offers opportunities for a number of new therapeutic approaches”, says Hak.
Scientific publication:
Jeffrey Momoh, Sjoerd Hak et al.: Intravital microscopy for real-time monitoring of drug delivery and nanobiological processes. In Advanced Drug Delivery Reviews, October 2022.