In medical research, replacing animal testing with new and alternative tools, does not only minimise animal cruelty but also provides many benefits for us humans. Importantly, in addition to sparing the lives of the animals, it puts the physiology of the human body in focus.
Human and animal physiologies share some similarities but are also inherently very different. To predict how new drugs and medical products will behave in the human body, we are now conducting experiments using new tools called in vitro microphysiological systems. In vitro is Latin for ‘in glass’, and refers to experiments carried out in a laboratory, outside the body itself. In medical research, the use of such tools is dependent on regulatory approval processes pursuant to provisions stipulated by the Norwegian and international authorities; and on the other hand, on the development of new technologies and materials that enable us to conduct more physiologically correct experiments on cells and tissue in a laboratory.
As research scientists at the SINTEF MiNaLab, this is what we work with every day. In our laboratory, we work with technologies at micro-level. We manufacture the so-called microfluidic chips that biologists can use to cultivate and conduct experiments with cell cultures at micro-level. These technologies offer us new opportunities to study diseases and test new treatments in the laboratory. But they also present us with new challenges. One limiting factor is that the materials used to make microfluidic-based research tools do not always enable us to recreate physiology exactly as it is in nature, and this prevents us from mimicking the real physiological conditions we need for long-term cell cultivation and observation.
Oxygen, for example, is a key factor in this type of work. Oxygen is crucial to almost all living organisms. It drives the chemical conversion of food into the energy that living cells need to thrive and grow. However, inadequate levels of oxygen can activate unwanted physiological processes which, if they persist, can result in cell mortality. For this reason, relevant in vitro models of human physiology will always require tools that make it possible to fix and control oxygen levels for several days while the material is being handled and analysed.
In our laboratory, we work with technologies at micro-level. We manufacture so-called microfluidic chips that biologists can use to cultivate and conduct experiments with cell cultures at micro-level. These technologies offer us new opportunities to study diseases and test new treatments in the laboratory.
At MiNaLab, we have accumulated a lot of experience in the design and manufacture of silicon, glass, and polymer microfluidic chips for cell manipulation. Working together with other researchers and industrial sectors, we see that there is an increasing demand for assembling chips made of many different materials, each with their own specific properties and functions. This serves to expand the total functionality of a given chip, reduces costs and at the same time enables us to focus on sustainability.
In one of our current projects, called ImmuneDroplets, we are developing tools that we can use to study the interaction between virus-infected lung cancer cells and a special type of immune cell that acts as nature’s own ‘killer’ cell. This research may contribute towards a better understanding of lung cancer and open the door to new treatment approaches. Our objective is to carry out modelling and experiments at both single-cell and cell population level, enabling us to highlight the benefits of using microfluidic tools for experiments of this type.
As part of this project, we have been testing a polymer called polymethylpentene (PMP) for use in long-term cell cultivation. This work has recently been published. This material attracted our attention because it offers a unique combination of physical and chemical properties. Nevertheless, we were unable to predict our results with any certainty because PMP has not been in active use in connection with in vitro microphysiological systems before now.
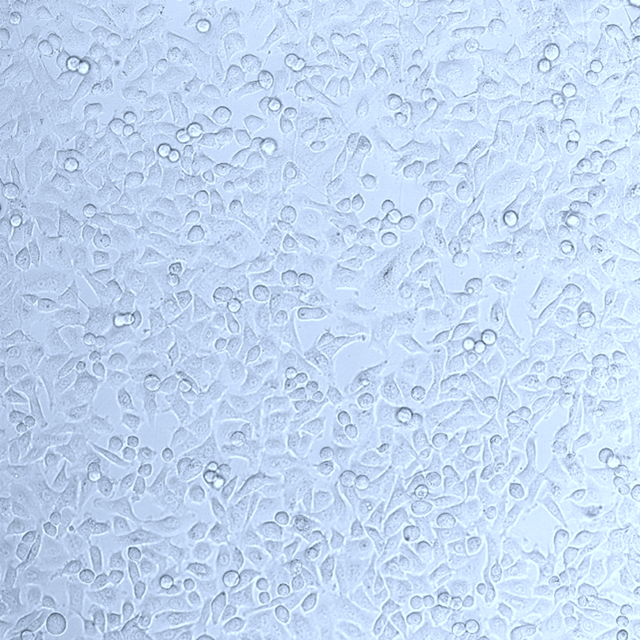
Adherent epithelial cells under cultivation in a microfluidic chip made of the polymer PMP. Photo: SINTEF
The findings we made are very promising. We found that PMP makes it possible to cultivate cells with an adequate oxygen supply in microfluidic chips for more than four days. We also observed that the material remained sufficiently rigid and transparent for high-resolution microscopy, while at the same time also withstanding the sterilisation regime.
In one of our current projects, we are developing tools that we can use to study the interaction between virus-infected lung cancer cells and a special type of immune cell that acts as nature’s own ‘killer’ cell.
PMP allows us to maintain adequate oxygen levels, comparable to the polymer polydimethylsiloxane (PDMS), which is the best-known gas permeable material currently being used in microfluidics. However, in contrast to PDMS, PMP is also rigid enough to be used to make robust thin plates. This makes it possible to carry out high resolution microscopic analyses that would normally be performed on cells cultivated on thin glass plates called coverslips.
The development of the prototyping methods using PMP is a collaborative effort between SINTEF Digital and SINTEF Industry. We are now hoping that our research results, together with new insights into all the beneficial aspects that PMP offers for in vitro microphysiological systems, will contribute towards the construction of reliable models of human physiology in the laboratory and help us to perform extended detailed studies of patients’ cells or tissue samples without the need for animal testing.
The project ImmuneDroplets is being carried out as part of the bilateral basic research programme GRIEG and has received funding amounting to €1.4 million from EEA/Norway Grants.



