Accident and Emergency (A&E) doctors are often young and inexperienced, with little knowledge or understanding of older patients. This means that patients may sometimes be misdiagnosed. Older patients could be admitted unnecessarily, admitted to the ‘wrong’ department, or discharged with a medical problem that has not been identified and treated. These findings are based on general observations made in a wide number of A&E departments.
St Olav’s Hospital, Vestfold Hospital, Trondheim municipality and SINTEF have all been involved in tackling the problem. They have obtained information from abroad, made observations and conducted surveys, and interviewed patients, relatives and staff.
On the basis of this information, Trondheim municipality and St Olav’s Hospital are now beginning to develop an improved A&E experience for older emergency patients.
A challenging patient group
When elderly people arrive at A&E, it is often because of an acute illness or accident. However, these patients may have complex symptoms, including chest pains, stomach pains, a tendency to fall, cognitive impairment, dehydration and movement problems. And it is often not the most visible symptom in the elderly that is the most important in the sequence.
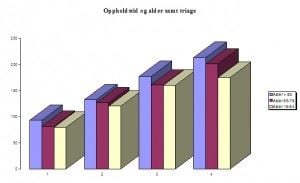
Statistics from St Olav’s show that it takes longer to determine which is the most important symptom to treat in older patients than in younger patients.
Click to open
Up to 40 percent of older people who come to hospital may be suffering from delirium, and may find a stay in hospital such a strain that this condition becomes worse.
Older people also have problems finding their way around a hospital: Signage may be poor, clocks too small, and in rooms without windows and adequate lighting, patients may lose track of whether it is day or night. It can also often be difficult to have a confidential conversation in A&E.
Enthusiasm and preliminary project
Senior Adviser Espen H. Aspnes is the innovation consultant for InnoMed in Central Norway. He tells the story of the American ‘geriatrics guru’ Dr. Bill Thomas, who started off the whole thing. Thomas started his medical career in A&E, and quickly confirmed that they were not well designed for older patients. His work resulted in changes to the A&E departments in a number of American hospitals.
“We have invited Bill Thomas to Norway to present workshops on two occasions. Both times, his message created a great deal of interest and enthusiasm”, says Aspnes. “The participants have understood that in order to provide older people with good treatment that is suitable and safe, it is essential that we have sufficient experience and knowledge about them”.
So great was the interest that Senior Consultant Jostein Dale of St Olav’s Hospital decided to take this a step further. He and Aspnes submitted an application for a preliminary project. The objective was to acquire enough knowledge to be able to create an A&E department designed for older people. The preliminary project ‘A&E for the elderly’ began in 2012.
Visual studies of activity and patient progression
“An A&E department has a complicated structure, with several processes going on in parallel”, says Aspnes. “This means that our work as service designers has been absolutely crucial. Using a method known as ‘Service Blueprint’, we create a diagram that visualises the services and progression experienced by a patient in the department”.
Espen Aspnes shows us the diagram, which is made up of parallel horizontal lines in different colours.
• A green line shows the progression through the A&E ward, as perceived by the patient.
• The red line shows the physical locations that the patient has experienced (rooms, transfers, access to technical aids, lighting, signs).
• The blue line describes the encounters the patient has had with staff.
• And an orange line shows what happens ‘behind the scenes’ – things the patient doesn’t see.
“The weaknesses in the system become very clear”, says Aspnes. “One of things that the diagram shows us is how time-consuming the latter activities are. Registration takes a long time, because Norwegian hospitals have several parallel IT systems, and unfortunately the elderly person has to repeat their medical history several times to different people”.
FACTS:
- The American 'geriatrics guru' Dr Bill Thomas became the key that inspired hospitals to do something about A&E and the elderly in Norway. Bill Thomas is internationally renowned for his new methods of providing care for the elderly. ('The Eden Alternative').
- As part of the InnoMed preliminary project 'A&E for the elderly' (2012–2013), St Olavs Hospital, Vestfold Hospital, Trondheim municipality and SINTEF have prepared a report. This has provided a basis which is being used to improve the situation for elderly people in Accident and Emergency departments.
- As a continuation of this, service designer Hanne Ekran Thomassen at SINTEF has made a study of the current Emergency Medical Centre in Trondheim.
- Trondheim municipality has now started a major project that will continue until 2017 and involve the 'Helsevakta' and the Emergency Medical Centre of the future. St Olav’s Hospital, Trondheim municipality and SINTEF are working together. Their objective is to develop a coordinated patient experience for elderly Accident and Emergency patients when the municipal Emergency Medical Centre is moved out of the hospital.
Major potential for improvement
The A&E department at St Olav’s Hospital moved into new premises in 2011. They will now use the results from the preliminary project to improve their procedures and their current physical surroundings.
Vestfold Hospital is going to build a new A&E department using the results in its planning work, and Trondheim municipality is about to develop a new Emergency Medical Centre that will be separate from the hospital. The municipality is working with St Olav’s Hospital to improve the total patient experience for the older emergency patient.
“St Olav’s has come a long way with its A&E skills, but the physical surroundings are still not optimum”, says Espen H. Aspnes. “However, when Trondheim municipality moves its Emergency Medical Centre, this could give it space to make improvements in its A&E department”.

