Currently, when we give our doctor a blood sample for a ‘full check’, it can only be analysed for five or six indicators, such as blood percentages, blood sugar and infections. For other test results, the sample must be sent to a central laboratory for analysis.
Improved sensitivity
Four years ago, SINTEF began a joint project with Stanford University in the USA and the University of Oslo (UiO). The aim was to build a sensor that could improve sensitivity a million fold, making it possible to measure individual particles in the blood, including proteins at extremely low concentrations, as well as DNA and RNA (ribonucleic acid) molecules.
The result is a new nanoparticle sensor developed in MiNaLab in Oslo.
Photonic crystal
The sensor comprises a thin silicon membrane – about three hundred times thinner than a single hair. It is perforated with hundreds of small holes arranged in a regular pattern.
‘We call these structures photonic crystals’.
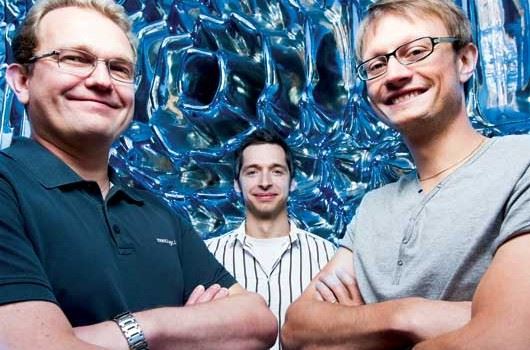
The same structures occur naturally in the wings of some butterflies,’ says Ib-Rune Johansen at SINTEF ICT. Like his colleagues Jon Olav Grepstad and Michal Mielnik, he believes that they are not exaggerating when they claim that this is “the ultimate bio-sensor – at the cutting edge of nanotechnology”.
Starlight
One of the properties of the crystal is that it amplifies parts of the light spectrum.
‘When we are looking for particles in blood samples, we illuminate the photonic crystal from behind. That way, we can amplify the intensity of light within the membrane by many hundred fold. The crystal is impervious to light: all light is reflected and nothing gets through. Viewed from behind, therefore, the crystal looks like the dark night sky. However, each particle that is captured becomes trapped in a hole in the membrane and allows some light to leak through – giving it the appearance of a star in the sky,’ says Johansen.
‘Our breakthrough came with this opportunity to see these microscopic particles,’ he tells us.
Early cancer diagnosis
Currently, medical laboratories measure proteins to detect imbalances in the body that occur when an infection is present. The new sensor can take these analyses much further.
SINTEF’s chemists are trying to attach receptors to the wall of each of the perforations in the membrane (biofunctionalisation). When blood is pumped through, the receptors trap very specific molecules, depending on what the scientists are looking for. Because the sensor/membrane has many perforations, they can specify a wide range of different proteins. It will thereby be possible to detect illnesses such as prostate and ovarian cancer in their very early stages.
Two challenges overcome
Work on biosensors faces two challenges. The first is to make the sensors sufficiently sensitive. The second is to ensure that they measure what they are supposed to measure. The sensors must also be able to differentiate between two particles, and select only those particles that have been specified (specificity).
The SINTEF researchers have improved their sensor’s sensitivity a million fold compared with ordinary sensors. They can now measure particles down to 20 nanometres.
‘Many proteins relevant to diagnosis are in this size range, but many others are even smaller. We can currently detect individual molecules of the larger proteins. We can also detect smaller protein molecules, but not individually, i.e. we need more protein molecules before we can detect them with our sensor. However, the aim is to perfect the sensor’s architecture so that in the long term we will also be able to detect individual molecules of even the smallest proteins,’ says Michal Mielnik.
The researchers have also discovered a high specificity method, as well as their exceptional specificity method. Patent applications have been filed for both discoveries.
Sensitive – and cheap
‘We are very optimistic. So far, we have succeeded with-out a lot of support. However, a great deal of research remains to be done. In order to develop an industrial product, we need assistance from the Research Council of Norway and the EU,’ says Ib-Rune Johansen.
In the autumn, they will run artificial blood samples through the membrane, and in the spring, they will run tests using proteins from ovarian cancer.
Perhaps the best news of all is that it will only cost medical centres a few thousand kroner to buy the ‘tool’ – consisting of the sensor/membrane, a light source and a standard camera of the type used in mobile phones and PCs.
As well as its impact on medicine, the sensor is likely to make it possible to count and define limits for naturally occurring harmful nanoparticles. It will be possible to monitor the quality of water, air and food.
Åse Dragland