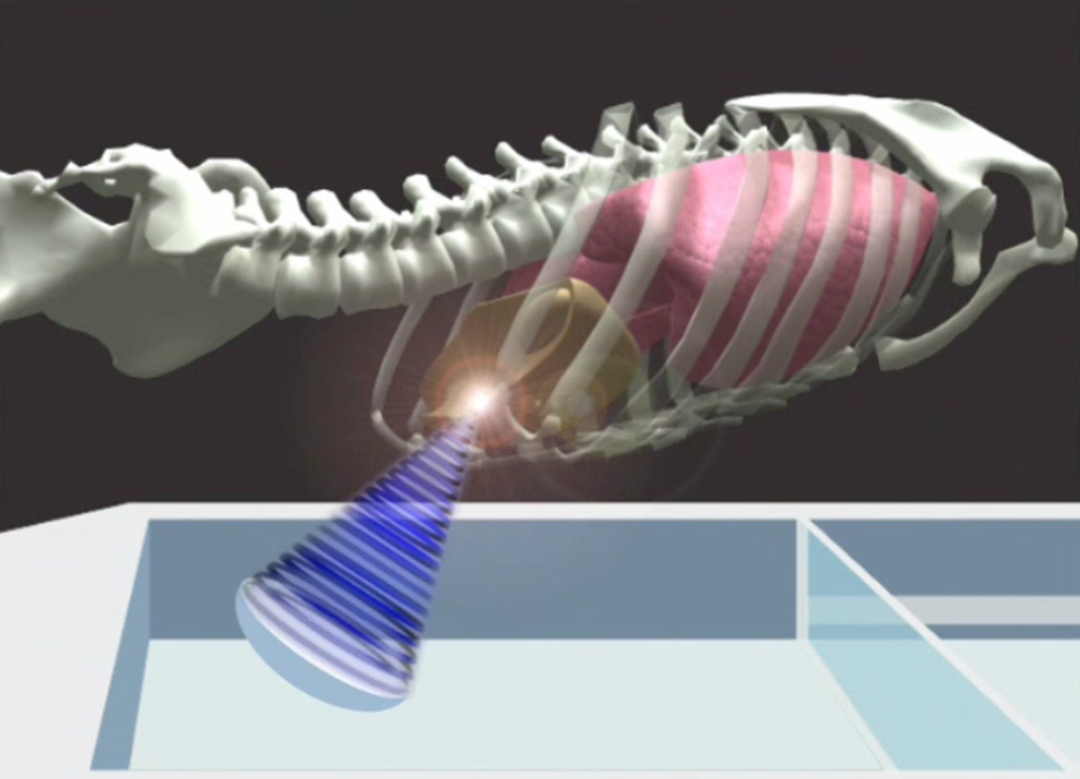
Although it might sound like science fiction, the following scenario could soon become reality: an elderly man has a lethal tumour of the liver, which cannot be operated on in the normal way. The tumour is too close to major blood-vessels, and it is not certain that the patient would survive such a serious operation. Instead, he is placed in a magnetic resonance (MR) apparatus and a large ultrasonic probe is placed on his abdomen. Within a few seconds, three-dimensional images of his abdominal cavity and liver appear on the computer screen. With millimetre accuracy, the doctors set up a therapy plan that will transmit high-intensity focused ultrasound into the tumour with the aid of the large ultrasound probe and the 3D MR map. When they press the button, ultrasound generated by several hundred elements is focused into the tumour, heating the spot to 85o Celsius, until all the cancerous cells are destroyed. In a few minutes the operation is over, and the patient can get up and walk out of the operating theatre.
Moving goals
“The story of this man is far from being a fantasy, in that it is based on clinical trials that have been carried out in a hospital in Rome,” says SINTEF project manager Thomas Langø, who has been collaborating closely for several years on image-guided surgery and ultrasound with surgeons at St. Olav’s Hospital in Trondheim. Now, he and his colleagues will further develop the system, which goes by the name of MR-guided Focused Ultrasound Therapy (MRgFUS). They hope to improve the method sufficiently to enable it to remove tumours in organs that are mobile during the treatment.
“When the heart is beating and the patient is breathing, the soft organs in the abdominal cavity, such as the liver and kidneys, are in motion. This means that it is still difficult for surgeons to employ the new technology to accurately target tumours in this part of the body. For this reason, the method has so far only been approved for the treatment of benign tumours in the cervix,” says Langø. Researchers from ten European countries are going to do something about this in the course of the European Union’s FUSIMO project (www.fusimo.eu). The challenge lies in developing a tool that will enable surgeons to target tumours in moving tissue with millimetric accuracy and in real time.
SINTEF is leading efforts regarding the design and specification of the system in a clinical perspective, and is also involved in how we can track movements of the liver and kidneys during treatment using ultrasound.
“At SINTEF, we have been working for many years on ultrasound as a surgical imaging and guidance tool. This is a technology that is ideal to combine with high-intensity focused ultrasound as a method in therapy,” says Langø. We also have large datasets that describe the interior of the body and how various organs move within it. There are not many research groups in the world that can simultaneously image and track the movements of organs and tumours in the way that we do.”
4D ultrasound
What the SINTEF scientists want to do is to visualise and track the movements of soft tissue by means of 4D, i.e. three-dimensional images in real time.
“4D refers to 3D plus time,” explains Langø.
The work is being carried out in collaboration with a team of Italian doctors, and researchers from Scotland, Germany, Netherlands and Switzerland.
Langø says the challenge is similar to firing at a moving target, and it involves giving surgeons an imaging tool that will enable them to “hit” the moving object without a time delay. The system thus has to predict exactly where the part of the tumour marked for destruction will be a few milliseconds ahead in time. This has to be done several times until the whole tumour has been destroyed.
The initial aim is to create a simulator that will enable surgeons to test-operate “virtual” patients, which will show whether MRgFUS is the appropriate method for any given patient and tumour. If the simulated operation goes well, the patient can be operated “for real”.
Christina Benjaminsen